- Research
- Open access
- Published:
Investigating the learning value of early clinical exposure among undergraduate medical students in Dubai: a convergent mixed methods study
BMC Medical Education volume 25, Article number: 638 (2025)
Abstract
Introduction
The benefits of Early Clinical Exposure (ECE) in medical education are often stated but there is limited evidence on how to effectively maximize its learning value. The challenge for medical educators lies in finding ways to enhance the quality of ECE in alignment with students’ feedback, while realizing the learning outcomes. The purpose of this study is to investigate undergraduate medical students’ perception of an innovative ECE intervention in Dubai, United Arab Emirates, developed using design-based research in alignment with adult, experiential learning theories.
Methods
A convergent mixed methods study design was utilized. The data was collected using a tailormade survey to solicit both quantitative and qualitative feedback. Quantitative data was analyzed using SPSS. Qualitative data analysis was inductive based on constructivist epistemology. Following the conclusion of the independent data analyses of the quantitative and qualitative datasets, the primary inferences were integrated using the iterative joint display analysis process.
Results
Out of the 68 students who attended the ECE, 54 responded. The percentage of the total extent of agreement that the ECE: familiarized them with learning in the clinical environment and brought forth the institutional values were 79.60% and 86.43%, respectively. The extent of active engagement and self-directed learning, with a mean of 6.80(2.42), was significantly associated with how much the learners reaped from the learning experience (P < 0.05). A novel conceptual model, namely: ‘Early Clinical Exposure Added Value’, with five interconnected themes, was developed from the qualitative analysis. Integration of findings led to six meta-inferences: Embeddedness in context of learning, System perspective, Patient-centricity, Theory–practice link, Resilience, and Proactiveness.
Conclusion
The more medical students engage in their learning, the more ECE contributes to building their academic resilience, and propels them in terms of clinical correlations, skills’ development, and values reinforcement. Securing engagement opportunities for the learners, when designing and planning for the ECE, is essential. Optimizing the ECE learning value can happen systematically through continuously developing the respective intervention in alignment with the principles of design-based research and anchoring it in constructivism experiential learning theories.
Introduction
Health professionals continue to observe considerable changes in the nature by which health care is delivered [1, 2]. Historically, medical education has identified competences around core medical expertise. The Flexner report marked a constructive transformation in medical education, enabling medicine to become firmly rooted in biological science. It is believed, though, that the execution of the report’s recommendations contributed to the erosion of the societal perception of the physician as a ‘trusted healer’ [3, 4]. There is rising recognition that healthcare providers’ competences need to extend beyond medical sciences [5, 6].
Early clinical exposure (ECE) is a learning and teaching methodology which fosters the exposure of medical students to the patients as early as the first year of medical college [7]. It has been defined as authentic human contact in a social or clinical context that enhances learning of health, illness, and/or disease, and of the role of the health professional [8]. It is believed to provide a clinical context and relevance to basic sciences learning. It is also supposed to facilitate early involvement in the healthcare environment that serves as motivation and reference point for students, leading to their professional growth and development [7]. Several terms have been used interchangeably across the world to describe similar learning and teaching interventions, including but not necessarily limited to early patient experience, early patient contact, early integrated patient contact, early clinical experience, early clinical contact, early student-patient contact, early professional contact, and/or early patient encounter [9, 10]. ECE is increasingly recognized as a vital element of medical education, aimed at bridging the gap between theoretical knowledge and practical application, which could feed into circumventing the consequential drawbacks of the transformation that accompanied Flexner report along with maintaining its substantial benefits [3, 4]. ECE allows students to engage with patients early on in their educational journey. This has been proven to enhance the medical students’ understanding of the realm of basic sciences and its relevance to patient care [11, 12]. Students have reported increased motivation and comprehension after ECE, particularly in correlating basic sciences, like anatomy and physiology, with clinical cases [11, 13]. ECE enables the development of clinical skills and the understanding of patient-centered care [14]. A study comparing ECE with traditional teaching methods found that students exposed to ECE demonstrated superior performance in practical skills, such as blood pressure measurement, and developed a better understanding of the sociocultural context of diseases [15]. Medical students, in another investigation conducted in the Middle East, reported that ECE strengthened their understanding of the delivery of clinical care to patients and gained familiarity with the clinical environment. Most students attributed improvement in history and examination skills to the ECE [16]. ECE improves students'academic performance and communication abilities [17], fostering greater confidence in their roles as future healthcare providers [7, 15, 18]. Additionally, medical students have reported that ECE facilitated a clearer grasp of concepts and improved their doctor-patient relationships [19].
In addition to enriching the students’ learning experience, ECE prepares students for real-world clinical environments, thereby aligning educational practices with the demands of modern healthcare [13, 18]. ECE fosters a sense of professionalism and the development of students’ career paths [18, 20, 21]. Studies have indicated that ECE significantly improves students'knowledge retention of complex concepts, as evidenced by positive shifts in test scores [18, 22]. Furthermore, students have reported a heightened appreciation for the realities of clinical practice, with many advocating for more frequent and extended ECE sessions [12, 23]. Furthermore, ECE fosters the development of essential skills such as problem-solving and systems thinking, which are crucial for patient-centered care and understanding of healthcare structures [24].
The effective implementation of ECE in medical education comes with a range of challenges that, if addressed, could significantly enhance the learning experience for students. The lack of standardized ECE programs, insufficient clinical exposure opportunities, and the difficulty in integrating theoretical knowledge with hands-on practice are among those challenges. Other barriers to effective ECE implementation include medical students'heavy workloads, limited time for faculty to provide effective teaching, and concerns about patient confidentiality and safety, as well as cultural and environmental factors impediments [14, 16]. A cross-sectional survey conducted across European medical schools found that over half the respondents reported challenges in implementing ECE. These challenges included insufficient time within scheduled curricular activities, insufficient numbers of experienced faculty to accommodate the growing student population, resistance from senior staff regarding placements, and limited administrative support and knowledge [18]. Some studies suggest that despite ECE, medical students may still struggle with certain clinical skills, indicating a need for improved designing and planning [17]. Importantly, limited resources and time constraints in crowded clinical environments necessitate careful planning and faculty training to effectively integrate ECE into existing curricula [18, 25].
It is worth grounding ECE in adult, experiential learning theories. Several studies report on investigations around ECE that were designed in alignment with such principles [16, 26, 27]. Adult, experiential learning theories are based on the premise that adult learners are naturally motivated to develop, deploy self-directed learning [28, 29], and have mental models gradually built from previous experiences that take the form of a continuously developing resource for learning. These theories also assume that adult learners regularly exercise analogical reasoning in learning and practice, where they continuously identify similarities across situations or concepts to draw inferences and/or solve problems [30]. This is in congruence with the basis of Kolb’s experiential learning cycle [31, 32] which highlights that the learners reflect upon concrete, hands-on experiences to identify gaps in their mental models. They then engage in abstract conceptualization to adapt their mental constructs. Following that, the learners actively experiment using the continuously developing mental models in new experiences. Accordingly, this constructivist perspective portrays experiential learning as opportunities for active experimentation and growth [33]. This develops competencies which in turn modify behavioral patterns leading to long-term change in practices. Accordingly, Kolb’s experiential learning theory deepens the understanding around the individual-level growth that is occurring as the learner is going through hands-on experiences, however it leads to overlooking the fundamental development that is concurrently occurring in relating to others. The subsequent simplistic view of experiential learning pulls it away from its roots, where it was originally sourced from human relations’ training [34]. Cognition is thought to be influenced by the learner, the environment in which the learning is occurring, and the activity that the learner is involved in [35]. As such, it is important to conceptualize experiential education in more sociological terms, illustrating how the individual learner exists in relation to environmental factors, including cultural and social ones, and is continuously interacting with others [36, 37]. From a practical perspective, and to circumvent this limitation, when designing learning and teaching opportunities aimed at empowering medical students, it is worth considering Kolb’s experiential learning theory in conjunction with a social constructionism theory (where a small group of people learn through interacting with each other). This helps in leveraging the students’ embeddedness and their active participation in the context of learning towards maximizing the entailed learning [38].
Furthermore, rooting educational interventions in experiential learning models enables the contribution to the theory around the subject matter along with the provision of practical value (i.e., familiarizing medical students early on with learning in the clinical environment). Creating this parallelism between contributing to theory and to practice is actually one of the key characteristics of design-based research which is a method that allows for iterative investigations of the learning intervention in the authentic educational context [39]. These studies usually rely on mixed methods research design which enables the development of a systemic understanding of the subject matter, where students become participants in both the design of and analysis around the educational intervention [40,41,42]. Subject matter experts get to provide their feedback on the initial prototype of the learning intervention. Meaningful cross-disciplinary interactions between the involved designers, practitioners and/or researchers lead the continuous refinement of the initial design [43]. The evolving prototype gets continuously appraised by the involved stakeholders through interactive group meetings to integrate the lessons learned (in terms of the educational practice) and to advance the theories that the respective learning intervention is based upon (by virtue of its design). Accordingly, design-based research constitutes a valuable opportunity to improve both the practice and theory around educational interventions [44].
Although the benefits of ECE are frequently alluded to, there is limited evidence on how to effectively maximize its learning value towards preparing and maintaining humane and holistic future-ready health professionals [16, 45]. This is particularly relevant to ‘future-ready health professionals’ who are receiving their training in Dubai, United Arab Emirates (UAE): the most globalized country in the Middle East, according to an index that measures the economic, social, and political dimensions of globalization [46,47,48]. The challenge for medical educators lies in finding ways to enhance the quality of ECE in alignment with students’ feedback, while realizing the learning outcomes [26]. Accordingly, the overall purpose of the study is to investigate undergraduate medical students’ perception of an innovative ECE intervention, implemented in Dubai, UAE in alignment with adult, experiential learning theories, and continuously developing using design-based research. The mixed methods research design, adapted for the current study, was meant to answer the following three questions, corresponding (as per established mixed methods article reporting standards [49]) to the quantitative, qualitative, and integration elements, respectively (‘RQ’ stands for Research Question):
-
RQ1. To what extent do students consider that ECE have familiarized them with characteristics of learning and practicing in the clinical environment, and to bring forth the institutional values; and to what extent do they consider themselves to have actively engaged in their learning as part of ECE?
-
RQ2. What do students perceive the learning value of the ECE to be?
-
RQ3. How can the learning value of an ECE intervention be maximized?
Methods
Context of the study
The current study was conducted at Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU) in Dubai, United Arab Emirates (UAE) [50]. UAE is a multi-cultural, multi-ethnic setting in the Middle East and North Africa region, rooted in Islamic values and Arabian norms. UAE is a constitutional federation of seven emirates. Abu Dhabi city is the capital of the UAE federation [51]. Dubai is the largest and most populous of the seven emirates [47]. All UAE citizens in the seven emirates carry the unified nationality of the UAE, which is recognized internationally [51]. According to the Federal Competitiveness and Statistics Center, the UAE's total population (nationals and expatriate residents) was 9,282,410 in 2020 [52]. MBRU had set out, upon inception in 2016, to become an integrated academic health system, with clear articulation of its direction in the University’s inaugural goals (Appendix I: MBRU Inaugural Goals).
‘To advance health in the UAE and the region, through an innovative and integrated academic health system, that is nationally responsive and globally connected, serving individuals and communities.’
Today, MBRU is the implementation vehicle of two pillars (i.e., health professions’ education/‘learning’ and research/‘discovery’ arms) of the first integrated academic health systems in Dubai, namely: Dubai Health [53, 54] (Appendix II: Dubai Health Goals). Other than its ‘learning’ and ‘discovery’ pillars, Dubai Health oversees the operations of around 40% of the health sector in Dubai through its clinical enterprise (i.e., the ‘care’ arm). The rest of the health sector in Dubai is mainly privately owned and operated. Altogether, Dubai’s healthcare sector is regulated by the Dubai Health Authority (DHA) [55]. Besides, the ‘care’, ‘learning’, and ‘discovery’ arms, that can be mapped onto the traditional tripartite mission of the common academic health centers in North America [56], Dubai Health also has an arm related to philanthropy namely: ‘giving’. Dubai Health is characterized by a values-driven culture. The institution’s core value is ‘Patient First’. The other values are ‘Respect’, ‘Excellence’, ‘Teamwork’, ‘Integrity’, and ‘Empathy’. In addition to sharing its goals with Dubai Health, MBRU efforts align nationally with the Ministry of Higher Education and Scientific Research- Outcome-based Evaluation Framework [57] and internationally with the United Nations- Sustainable Development Goals (SDGs) [58] (Fig. 1).
Illustration of alignment of goals (micro-, meso-, and macro-levels). The figure shows how the pillars of Dubai Health (Care, Learning, and Discovery, and Giving) are feeding into the pillars of the Outcome-based Evaluation Framework (OEF) which in turn contribute to select Sustainable Development Goals (SDGs). Patient first, as the core value of Dubai Health [purposely located in the heart of the illustration, slightly towards the left (in Green, which is considered a balanced anchor for the other colors of the visible spectrum)]. This patient centricity is among the differentiators of MBRU from the rest of the Higher Education Institutions governed by the OEF of the UAE Ministry of Higher Education and Scientific Research
MBRU has three colleges, namely: Hamdan Bin Mohammed College of Dental Medicine, College of Medicine (CoM), and College of Nursing and Midwifery. One of the programs offered at CoM is the six-year Bachelor of Medicine and Bachelor of Surgery program (MBBS), which is built on a competency-based learning model. Queen’s University Belfast (QUB) [59] has been playing an active role in the quality assurance and maintenance of the MBBS, through a partnership with MBRU. This MBBS comprises three phases. The learning process is spiral [60]. The first year comprises Phase 1, where the students are exposed to basic concepts of medicine. Phase 2 covers the second and third years, where teaching is organized around body organ systems. The fourth through sixth years represent Phase 3 during which the students undertake their clinical clerkships in the public and private sector.
Phase 3 placements are undertaken in Dubai Health hospitals and clinics, and in the private Mediclinic Middle East (MCME) healthcare delivery network in the UAE. MBRU has had a public–private partnership with MCME since 2016 [61]. MCME has a capacity of around 1,000 inpatient beds and 1,300 doctors in the UAE, offering a full range of preventive and curative services, primary through quaternary. In the UAE, MCME has 7 hospitals, 3 of which are in Dubai, and 29 ambulatory care clinics of which 16 are in Dubai [48, 62]. In addition, MCME has been operating two standalone outpatient dialysis centers that offer public services as part of Dubai Health since 2021.
Description of the intervention
The ECE, reported upon in this study, was first offered in academic year 2023–2024, as part of a course named: Foundation of Clinical Medicine 2 (FOCM2) (Appendix III: Study Guide), which was delivered throughout the second year of the MBBS at MBRU. FOCM2 is part of a series of three courses (that were collectively overseen by R.A.J. at the time of this study), namely: Foundation of Clinical Medicine (FOCM). This series of three courses is offered in the first through third years of the respective MBBS (one course per year), that lay the groundwork of clinical skills, building the learner competence in a deliberate progression, prior to Phase 3 during which the students undertake their clinical clerkships (Fig. 2). It is worth noting that MBRU stakeholders identify the early clinical exposure among the unique attributes that sets its MBBS apart from other medical programs [50].
Each FOCM course is coordinated by a faculty member. FOCM2, which was coordinated by N.A.M. at the time of this study, is a clinical skills’ course that followed on from Foundation of Clinical Medicine 1 (offered throughout the first year of the MBBS). FOCM2 aims to enable students to effectively deploy clinical skills (e.g., medical consultations and physical examinations), maximizing the benefit for primarily the patients. The concepts introduced in FOCM2 are revisited and further developed in Foundation of Clinical Medicine 3 (offered throughout the third year of the respective program).
In the academic year 2023–2024, a total of 68 students were enrolled in the second year of the MBBS at MBRU. This cohort was from 19 nationalities (51 females and 17 males). FOCM2 was offered over 30 weeks, with two, two-hour classes every Tuesday (morning and afternoon sessions). The two sessions of the first week were integrated into the university orientation of year 2 students. For the second week, the morning session revolved around introducing the students to FOCM2 and to medical consultation. The afternoon session of the second week took the form of an induction to the ECE placements.
The remaining weeks took three forms. The first form of sessions, covering a total of seven weeks, was didactic where the students received two seminars per week of differing topics (one in the morning and the other in the afternoon on Tuesdays). The second form of sessions, covering a total of 15 weeks, was centered around practical skills development, offered in the Khalaf Ahmad Al Habtoor Medical Simulation Center at MBRU [63]. In these sessions, the 68 students were divided into two sections: each with 34 students. Each section of students took one of the two sessions (morning or afternoon), whereby the sequence of the two sections alternated. The clinical simulations were deployed in the morning session, where the section was divided into groups of 6 or 7 students (a clinical tutor, including N.A.M. and Q.Z., assigned to each group). The afternoon session was labeled as: ‘self-directed learning timeslot’, where the students had the liberty of choosing how they would like to invest their time towards meeting the course’s learning outcomes.
Every week, eight out of the 68 students were allocated to ECE placements during the ‘self-directed learning timeslot’. The development of ECE followed the principles of design-based research [39, 40]. The aim of the ECE was primarily to reinforce the students’ learning and to increase their motivation, better preparing them for the clinical phase of the MBBS and facilitating the transitions integral to it. This is achieved by familiarizing the students with the clinical real-life application of the theory they learn as part of the MBBS. The adapted design-based research relies on design thinking, which is a process that deploys a combination of innovation and creativity to iteratively develop, implement, and evaluate a novel learning and teaching intervention [43]. Through this approach, the study investigators: a group of medical education designers, researchers, and practitioners, strove to contribute to the advancement of knowledge in relation to the subject matter, while they are working towards improving the educational practice in the context of this study. The intervention, compounded with the associated research, took place in authentic, real-life settings, and was design driven [39]. It involved continuous cycles of design, evaluation, and redesign. Accordingly, the insights developed from evaluating the experience led to further improvement and redesign [44].
All the organization and administrative duties related to the ECE (including logistics and communications) were handled by a faculty member (Q.Z.). The last form of sessions, covering a total of six weeks, did not include any structured teaching; the corresponding sessions were either ‘peer-practice weeks’ (two weeks where the students, in groups, led practicing for their assessments) or ‘assessments’ (formative or summative, covering four weeks).
Each student enrolled in FOCM2 (i.e., 68 students) was required to participate in 2 ECE placement visits to healthcare centers in Dubai (i.e., a total of 136 ECE placements). The underlying assumption, in alignment with adult learning theory, is that the learners are self-regulated [28] and intrinsically motivated to learn from experiences [30]. The entailed learning facilitation was in alignment with Kolb’s Experiential Learning Theory [31], complemented by social constructionism theory [32, 33, 38]. The preset learning outcomes of the placements were for the students to:
-
Observe clinicians during consultation with patients.
-
Talk to patients about their illness and experience of healthcare (when possible)
-
Observe members of the multi-disciplinary teams during their interactions with each other and with patients
-
Reflect on their clinical experience as part of FOCM courses
Placements were complemented by structured consultation skills training in the simulation center as part of FOCM courses. The design of those sessions was based on theoretical and empiric research in adult and experiential learning, where the educators took into account the learners, their experiences, and the overall learning environment [30].
To organize for the logistics of the students’ allocation, a comprehensive list of the 68 year 2 students was obtained from the Student Services and Registration team at MBRU. The students were randomly allocated across three facilities (Fig. 3). The choice of facilities was driven by the fact that students were meant to observe generic skills, along with the perceived capacity and willingness of the facilities’ clinical teams to accommodate students. Accordingly, one of the three facilities included was a primary healthcare center in Dubai Health, offering diverse services. The chosen healthcare center was newly established at the time of the study with a prime location by the seaside (which was taken into account as a variable that would increase the pleasantness of the experience for the students). The other two facilities included were dialysis centers which are also part of Dubai Health, operated by MCME. The specialized clinics were included because they serve a pool of patients with chronic disease (kidney disease). This pool of patients remains relatively stable over time, and require ample care onsite in the centers from a multidisciplinary team covering an extensive array of generic services. All those aspects maximize the exposure and in turn the learning experience of the students.
Each week (for 15 weeks), a total of 9 students were allocated placements across the three included facilities (3 per facility, with minor exceptions to account for 2 placements per 68 students). The first placement visit took place on 19 th September 2023 and the last one was on 23rd April 2024.
Prior to the placements, the learning outcomes of the ECE in specific and that of FOCM2, in general, were shared with all healthcare providers at the three centers. Reminders about the ECE were sent (by Q.Z.) to the corresponding students and healthcare providers a day before the respective placements. Immediately after each placement, the students were asked to complete a form (Appendix IV: Reflection Form) that calls for reflecting upon the experience and documenting those reflections, followed by endorsement by the supervising healthcare providers.
Research design
A convergent mixed methods study design was utilized for the current study [64, 65]. This research design is encouraged in the research field of health professions’ education and is believed to enable the development of a holistic understanding of the topic under investigation [66,67,68]. Accordingly, quantitative and qualitative data were analyzed independently, and then the generated inferences were merged to result in meta-inferences using the iterative joint display analysis process [69]. The integration of generated information is believed to raise the reliability of the study [70].
The current study adhered to the Declaration of Helsinki. Ethical approval was granted by two relevant research governing entities: Institutional Review Board of MBRU (MBRU IRB- 2024–20) and Dubai Scientific Research and Ethics Committee (DSREC) at the DHA (DSREC-GL14 - 2024). An electronic informed consent (following the same established guidelines of written informed consent) was obtained from all participants prior to participating in the research study (i.e., providing their quantitative and qualitative feedback on the respective learning experience).
Data collection
The data was collected using a survey (in English language, as per the language of MBRU day-to-day instructions) designed specifically for the purpose of the current study (Appendix V: Data Collection Tool). Participants'anonymity, confidentiality, and privacy were protected. The survey aimed at capturing the students’ perception of ECE. It was designed to solicit both quantitative and qualitative feedback, taking into account the need to efficiently obtain data to avoid burdening the students. Although surveying is considered more rigid than other data collection mechanisms [71], the constancy of the data collection tool and process enabled standardization. Even though the tool entailed open-ended questions, relying on surveys to capture narrative data minimized subjectivity [72]. It is a convenient data collection tool that is cost-effective and enables securing a good response rate [73].
The survey was composed of six sections. The first section included a single open-ended question which inquired about the students’ understanding about ‘Learning in the Clinical Environment’, in the broadest sense. The second section included a five-point Likert-type scale (of 15 components) that measured the students’ extent of agreement that the ECE familiarized them with 15 preset characteristics of learning in the clinical environment (i.e., ECE Familiarization tool) (Table 1). The third section also included a five-point Likert-type scale (of 6 components) that measured the students’ extent of agreement that the institutional values were evident in their clinical placement (as part of the ECE) (i.e., Visibility of Values tool) (Table 1) [54]. The fourth section was again composed of a single open-ended question that solicited the students’ point of view of the immediate effects and longer-term impact of the ECE on them and their peers. As for the fifth section, it was a Net Promoter Score® to capture the extent to which the students’ considered themselves to have actively engaged with this ECE and deployed self-directed learning to maximize its learning value [0 to 10 scale (0: Not at all- 10: To the furthest extent)], followed by an open-ended question where students were asked to provide an explanation of their rating to the preceding question. The sixth and final section was composed of two open-ended questions, probing the students to highlight strengths of the ECE and suggest ways to improve it.
The tailormade survey underwent two validation phases. Firstly, two faculty members, one from each of basic and clinical medical sciences departments within CoM at MBRU, were contacted for the content validity. Secondly, the questions of the generated tool were discussed with two clinical tutors to assess the clarity, comprehensibility, and readability of the questions and the flow by which they are presented (i.e., face validity). Accordingly, the open-ended questions got minorly modified to enhance readability. In addition, two components were added to the ECE Familiarization tool, namely: Hygiene and infection control practices, and Documentation (i.e., Electronic Medical Record keeping). The electronic survey was administered (using a feedback analytics platform named: Blue, provided by Explorance inc.© [74]) in January through April 2024 following the second ECE placement for each student via a software that automates and analyzes feedback processes [75] managed by the Institutional Research pathway of the Strategy and Institutional Excellence (SIE) unit at MBRU. Accordingly, the students received an invitation email, with a hyperlink to the survey, from the SIE team (generic email: yourvoiceisheard@dubaihealth.ae), followed by two reminders (one week apart). The survey stayed open for a duration of one month after second placement for each student. During this time, the survey was also accessible via the students’ Learning Management System.
Students provided their informed consent for participation. An information page appeared when the participating students clicked on the survey link embedded in the invitation email that they had received (before they started filling in the survey) that indicated to them that their participation is completely voluntary, and that their privacy and data confidentiality would be protected. No personal identifiers were recorded. Each participant was serially assigned a unique identifying number (1 through 54).
Data analysis
Quantitative
The quantitative data were analyzed using SPSS for Windows version 27. The descriptive analysis consisted of computing overall extent of agreement score for the 15 components of the ‘ECE Familiarization’ tool and another score for the six components of the ‘Visibility of Values’ tool. The mean and standard deviation for the overall scores of both tools and for each of their components, and that of the ‘extent of active engagement and self-directed learning’ were calculated. The validity tests of Cronbach’s Alpha, and the Principal Component Analysis (PCA), accompanied by bivariate analysis, were performed to assure the internal consistency and external variance, respectively, of the ‘ECE Familiarization’ and ‘Visibility of Values’ tools.
To select the appropriate inferential analysis tests, a test of normality was conducted for both of those scores and individual component of theirs, and that of the ‘extent of active engagement and self-directed learning’. The data were all found to be not normally distributed. Accordingly, Kruskal–Wallis one-way analysis of variance test was used to assess the potentiality of associations between the following variables: ‘ECE Familiarization’ and ‘Visibility of Values’ (overall scores and individual components), and ‘extent of active engagement and self-directed learning’.
Qualitative
The qualitative data analysis was inductive and began after the conclusion of the data collection. All the narrative data collected through five questions were consolidated into a single database. The iterative analysis process was based on constructivist epistemology [76]. This was done using a phenomenological, participant-focused approach to thematic analysis by four data analysers (R.A.J., N.A.M., F.O., and Q.Z.). Before the analysis, the four researchers proactively identified personal characteristics that they collectively think may influence their perceptions in relation to the subject under investigation. One of the data analysers (F.O.), who has developed expertise in conducting qualitative socio-behavioural research, assured the rigor of the deployed analytical framework through ensuring the consistent application of the underpinning assumptions and theories. By displaying rather than avoiding the investigators’ orientation and personal involvement in the research and by evaluating interpretations according to their impact on participants, investigators, and readers [77], the quality control exercised in this investigation shifted from the objective truth of statements to understanding by people. This interpretative approach involves the ability to acknowledge and recreate the experiences of the participants, which differentiates it from standard scientific inquiry. The purpose of this technique is not to find casual explanations but rather to understand and relate to participating individuals, and their thoughts, motives, and actions. This methodology assumes that researchers can interpret individuals’ thoughts, emotions, and behaviours by genuinely understanding their self-expressions.
The adapted qualitative analysis followed the Braun and Clarke six-step framework [78]. This multi-phased approach to thematic analysis is widespread and has been encouraged in research around health professions’ education [67, 79,80,81]. NVivo 15 [82] was relied on to assign codes to the categories and themes, and in turn facilitate the categorization of the text fragments highlighted by the data analysers.
The analysis process is described by the following steps:
-
1.
Familiarization with the data. The data analysers (R.A.J., N.A.M., F.O., and Q.Z.) took turns in reading out loud the essays to familiarize themselves with the compiled dataset. They thoroughly reflected upon the content of the de-identified data, sharing any thoughts that surfaced for them.
-
2.
Generation of initial codes. Text fragments from the qualitative dataset that related, directly or indirectly, to the overall objective of the study were extracted. Accordingly, any text segment relating to the participants’ perception of the ECE was tagged. This process kept going until data saturation was attained and no new insights were observed in the dataset. This methodical review led to the development of categories of text fragments which paved the way for the next step.
-
3.
Searching for themes. This step involved conducting several rounds of structured reflections. As such, the various ways by which the identified categories could relate to one another were identified (leading to multiple potential interconnections). Any disagreement between the data analysers was perceived as an opportunity to reinforce the common ground between them, which is favoured in qualitative research [66, 83]. Accordingly, at any discordance, the discussion was pursued until a consensus was attained.
-
4.
Reviewing themes. The categories were gathered to form higher-order themes, according to the linkages that made most sense to the four data analysers (Fig. 4).
-
5.
Defining and naming themes. Each category and theme were assigned a code and defined in the context of the study, leading to the creation of the study’s conceptual model. A respondent validation followed. Randomly selected participants were invited to a virtual discussion. In this meeting, the principal investigator (R.A.J.) guided attendees through the research questions, the qualitative analysis process, and the generated conceptual model. After considering how well their survey responses aligned with the model, the attendees agreed with all the identified codes and how the model illustrated the connections between categories and themes.
-
6.
Reporting on findings. The results of the abovementioned steps were narratively reported (i.e., results section) in alignment with established guidelines, including the Standards for Reporting Qualitative Research (SRQR) [34, 49, 83, 84]. To further substantiate the findings, a tally was conducted. The four data analysers reported on the number of analysed text segments within each category. If for a single participant, more than one relevant text fragment was put in the same category, they were all collectively considered as one entry. Accordingly, the tally reflected the number of participants that brought up matters relevant to each of the categories.
Mind map deployed as a tool to facilitate the qualitative analysis. This figure is meant to demonstrate a steppingstone in the analysis process. The output of respective analysis is Fig. 5
Integration
Following the conclusion of the independent data analyses of the quantitative and qualitative datasets, the primary inferences were integrated using the iterative joint display analysis process [27]. This stage allowed for the generation of meta-inferences. In alignment with the guidelines of reporting on mixed methods research that were adhered to for the current study [49], the output of the integration was meant to address the third research question inquiring about the means by which the value of ECE can be maximized. The generation of meta-inferences enabled the researchers to identify where the findings build upon (or at least confirm) each other, as well as where they contradict each other.
Results
Out of those 68 students, 54 responded (i.e., response rate = 79.41%).
Quantitative
The reliability score of Cronbach’s Alpha for the ‘ECE Familiarization’ tool was 94.90%. The percentage of the total extent of agreement of ‘ECE Familiarization’ score was 79.60%, as per Table 1. According to the PCA (Kaiser–Meyer–Olkin Measure of Sampling Adequacy), 82% of the variance can be explained by the instrument (p < 0.001). Along the same lines, the Bivariate Spearman Correlations showed how the changes in the ‘ECE Familiarization’ score can be explained by changes in all fifteen components. Moreover, all components were associated with each other (p < 0.05).
The reliability score of Cronbach’s Alpha for the ‘Visibility of Values’ tool was 92.60%. The percentage of the total extent of agreement of ‘Visibility of Values’ score was 86.43%, as per Table 1. According to the PCA (Kaiser–Meyer–Olkin Measure of Sampling Adequacy), 88.40% of the variance can be explained by the instrument (p < 0.001). Along the same lines, the Bivariate Spearman Correlations showed how the changes in the ‘Visibility of Values’ score can be explained by changes in all six components. Moreover, all components were associated with each other (p < 0.001).
As for the ‘extent of active engagement and self-directed learning’, the percentage of the total average was 68%, as per Table 1. The ‘extent of active engagement and self-directed learning’, with a mean of 6.80(2.42), seemed to be significantly associated with both the ‘ECE Familiarization’ and the ‘Visibility of Values’ scores (P < 0.05). The ‘extent of active engagement and self-directed learning’ also seemed to be significantly associated with the following components of the two tools: Learning in the clinical environment, Health system functioning (e.g., settings of care, patient journey, and integrated care), Professional identity of healthcare providers, Importance of certain competencies (i.e., knowledge, skills, and attitudes) for clinical care among healthcare providers, Pressures on healthcare providers, Patient perspective of health and illness, and Hygiene and infection control practices, and Integrity and Empathy (P < 0.05).
In relation to ‘ECE Familiarization’ score, it seemed to be associated with ‘Visibility of Values’ score and all its components (P < 0.05). Besides its significant association with ‘Visibility of Values’ score, ‘ECE Familiarization’ turned out to also be significantly associated with all the ‘Visibility of Values’ score components (P < 0.05). As for ‘Visibility of Values’ score, besides its significant association with ‘ECE Familiarization’ score, it was significantly associated with all its components (P < 0.05), except for: Documentation (i.e., Electronic Medical Record keeping) (P = 0.21).
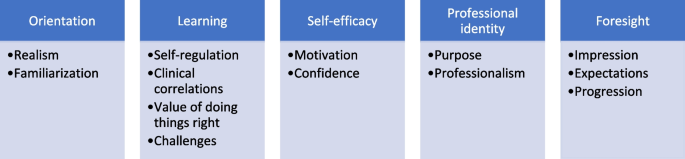
Qualitative
The qualitative analysis led, as per this study’s conceptual model: ‘Early Clinical Exposure Added Value’ (Fig. 5), to five interconnected themes, namely: Orientation, Learning, Self-efficacy, Professional identity, and Foresight. Within Orientation, two categories were identified: Realism and Familiarization. Within the second theme: Learning, the following four categories were identified: Self-regulation, Clinical correlations, Value of doing things right, and Challenges. Within the third theme: Self-efficacy, the following two categories were identified: Motivation and Confidence. As for the fourth theme: Professional identity, it encapsulated: Purpose and Professionalism. Lastly, within the fifth theme: Foresight, the following three categories were recognized: Impression, Expectations, and Progression.
The tally of the count of participants that brought up matters relevant to each of the categories showed the distribution, outlined in Table 2.
Orientation
This theme included any text fragment that reflects how the learning experience made the students more acquainted with learning and practicing in the clinical environment.
Realism
This category encapsulated all the text fragments that show the students’ perception of how this learning experience, which goes well beyond the classroom setting, embedded the students in the authentic context of learning.
15: ‘…realistic depiction of what happens usually in a hospital setting…’
40: ‘…it helped us learn things that cannot be taught in class…’
According to the students, the experience offered them a ‘reality-check’. They frequently described it as ‘novel’.
36: ‘…interactions with real patients and observations of real procedures…’
A few students considered the experience a pleasant change of setting.
22: ‘…also it was fun to go to a hospital, it was a ‘change of air’ to have in the middle of the academic semester…’
34: ‘…a positive change in the environment coupled with a fun, meaningful experience…’
Among the characteristics that stood out to the students the most in the clinical environment was the shared decision making between the healthcare providers and the patients. They seemed to recognize instances where healthcare providers strove to maximize their engagement with patients.
10: ‘…understand treatment options differ; it becomes more about making decisions with the patient…’
It seemed that the ECE brought to the attention of the students the sophistication of the practice of medicine. Several students highlighted the uncertainty and relativity integral to this practice.
28: ‘…applying it in a real-life scenario is not always as simple and straightforward…’
48: ‘…one thing I learnt is that there are no absolutes, white or black, ‘definite’ areas in medicine. There will be instances where one thing accommodates for another or compensates for it, and that is normal. This again confirms the widely circulated phrase in the field of medicine: ‘one size does not fit all’…’
Familiarization
This category included all the comments that show an increase in awareness about the characteristics of learning in the clinical environment. Students seemed to recognize distinct attributes and also reflected on how those features are interconnected which is essential for the functioning of the health system, emphasizing that ‘the whole is more than the sum of its parts’.
8: ‘…introducing students to other clinical settings like triage rooms or emergency departments where they will be more likely to interact with patients and view integrated healthcare in action….’
44: ‘… seeing the operations of different elements of the healthcare system and how these different elements interact…’
Among the attributes that they indicated were ones related directly to the placement site in which they were present for the learning experience. Many of the students reflected upon the logistics of commuting to and from the placement sites and their preferences in that regard.
8: ‘…familiarizing ourselves with the commute…’
The students also highlighted attributes related to the people within the placements.
1: ‘…interacting with patients and learning through observing physicians…
The ECE seemed to have increased their awareness of the patient perspective, and the healthcare providers’ roles and responsibilities.
5: ‘…I have a greater understanding of the patients’ perspective as I progress through my medical learning…’
They noticed the (often competing) pressures on the healthcare providers. The learning opportunity also shed light on several aspects of the patient-healthcare provider interactions, which include communication, privacy, and confidentiality.
9: ‘…exposes me to how health professionals interact with the patient…’
The means by which the healthcare providers conducted themselves was also apparent to the students, where the students either knowingly or otherwise pointed out embodiment of one or more of the institutional values.
15: ‘…gaining knowledge on how to act in a hospital setting (e.g., interaction between colleagues and with patients)…’
37: ‘…it was a good introduction to the clinical setting; we observed different departments and saw how they worked together to realize the value of patient first…’
It seemed that the ECE enabled the students to attribute a meaning to the term: ‘professional identity’, which they have been conceptually learning about for some time. They also saw firsthand the interprofessional teamwork that takes place in the clinical setting.
37: ‘…I enjoyed our discussion with a physician about the roles of different people that work together to rescue a patient in an emergency situation…’
48: ‘…appreciating how different things usually run in a clinical setting (e.g., patient-doctor interaction and interprofessional teamwork)…’
The ECE also brought to the attention of the students the workflow within the clinical setting and factors that affect it.
43: ‘…exposing us to …how health care is provided to the patients from the moment they enter the clinic until they leave…’
Several students also mentioned either directly or indirectly policies and procedures, including those related to documentation, and hand hygiene and infection control practices.
21: ‘…getting familiar with the system and knowing what is expected of me (e.g., how to handle situations and maintain patient confidentiality)…’
37: ‘…I observed a nurse communicate and take vitals from a patient. She then talked me through the documentation process and discussed with me how this information would reach the physician…’
Learning
This theme included the students’ reflections on the personal and/or collective growth that they experienced through observing in the clinical setting as part of the ECE.
Self-Regulation
This category highlighted the students understanding of self-directed learning.
42: ‘…like one of the doctors mentioned in the foundation of clinical medicine course: ‘you have to go out and look for medicine, it will not come to you’. I made sure to take full advantage of this opportunity…’
Being proactive through asking and answering questions, and through attentively listening were identified as key ways by which the students considered themselves to have engaged in their own learning. The students frequently highlighted incidences where they interacted with the healthcare providers, who served as educators in the authentic context of learning.
14: ‘…I was answering questions asked by the doctor and asking questions when I had ones…’
20: ‘…I tried my best to engage with the nurses and doctors, and to listen to the patients as much as I can.
Some students reflected upon how they prepared for the respective learning opportunity.
15: ‘…prior to entering the center, I tried utilising various resources to understand how dialysis works and review previous content relevant to kidneys and their physiology…’
Other students managed to get involved in the provision of care and not solely observe it.
24: ‘…I put in effort by asking questions and engaging with the staff. I also helped with taking history of patients, and taking the initiative, at one point, to bridge the language barrier between the provider and a patient…’
For students, taking an active role in their own learning had two prerequisites. Firstly, they seemed to recognize that they need to ‘step out of their comfort zone’, and to demonstrate proactivity, as well as (a degree of) adaptability.
1: ‘…I have actively engaged to maximize my learning in the clinical setting…’
15: ‘… see how knowledge can be applied in the clinical setting… find gaps in our current knowledge base, and what is needed to bridge these gaps to reach the expected performance…’
Some students even mentioned the value of developing plans and exercising particular learning strategies. Relevant to those examples, the students seemed to believe that the opportunity to maximize their learning lays within their control.
18: ‘…seeking out opportunities and leveraging self-directed learning strategies that maximize the educational value of the exposure…’
Several students appeared to be fairly assessing the extent of proactiveness that they deployed, where they reflected on whether they could have ‘done a better job’.
12: ‘…I think I could have better communicated and found a way to be more helpful in the setting and tried to ask more questions…’
23: ‘…I could have asked more questions…’
Those students seemed to assign value to their curiosity and hold themselves accountable to their own learning, where some of them highlighted their nervousness as a factor that held them back from learning during the placement.
20: ‘…I was curious to learn about the patient cases, and to figure-out whether, or not, I have studied them in the past year and a half…’
44: ‘…I could have engaged more actively with the consultation... I was asked whether, or not, I wanted to take history, but truthfully, I was feeling nervous, thought I would be more comfortable to stick to just observing the consultation…’
Secondly, the students seemed to believe that the opportunity for engagement must be present; proactivity alone is not enough. They highlight that the required opportunity for engagement is determined by factors outside their control, including the attitudes of and dynamics with healthcare providers, as well as the activities within the clinic, such as patient flow.
20: ‘…some nurses or doctors were not sufficiently engaging…’
47: ‘…I tried my best to engage with the program, but I did not get the same energy back…’
This is where several students made suggestions of how the ECE can become more engaging.
43: ‘…a good way to improve the early clinical exposure would be to provide some more guidance about how to approach it and what to expect so that we do not get overwhelmed as it is the first time we get exposed to such an experience…’
Clinical correlations
This category related to the growing understanding, among students, of the relevance of the lessons taught in the classroom.
6: ‘…seeing how what we have learned in class applies in the clinical setting…’
17: ‘…connected what we are learning on-campus to real life…’
Many of the students’ comments were about how their observations in the clinical setting related to the curricular knowledge they have been acquiring. They saw how the theoretical knowledge is applied in the clinical setting.
44: ‘…to see how the theories and frameworks we learn in class can be translated into practice and applied in a clinical setting…’
45: ‘…I get to connect what I learn from books and lectures to real-life interactions with patients…’
At several instances, the students seemed to be comparing and contrasting learning environments, describing the placements as ‘richer’ relative to all that they experience on campus.
37: ‘…we are able to learn skills that are more difficult to grasp in a typical classroom setting; for example, how the healthcare team works together is best learned through observation of the team in action…’
42: ‘…much richer compared to theoretical knowledge learned in lectures…’
They considered the ECE to offer them opportunities to identify gaps in their knowledge and strive to bridge them.
12: ‘…A lot of things seem less sophisticated when written on/read from books, but seeing the same topics applied in hospitals and clinics shows a new perspective that can help a student feel more comfortable in their future practice…’
54: ‘…work on improving some of the skills that we learnt in the foundations of clinical medicine course …’
The students identified competencies that they may have acquired, some of which were intended, including soft skills, such as: communication, professionalism, and empathy.
13: ‘…contributes to improving communication skills… it is a form of professional development…’
18: ‘…it enhances communication skills, empathy, and the understanding of patient care…’
The students also highlighted other competencies which were not intended learning outcomes of the ECE, such as: pathological basis of disease.
7: ‘…in the placement at the dialysis center, we heard lung crackles and examined fistulas, and talked to multiple patients. The doctor gave us an explanation of chronic kidney diseases; it was very informative…’
10: ‘…helped me link the theory learnt to clinical presentations of patients…’
Value of doing things right
This category related to text fragments that show the importance that the students attributed to certain competencies that they observed during the ECE, and how those competencies, according to the students, make the patients feel valued.
12: ‘…I now know what practices contribute to providing better services to patients…’
27: ‘…how important it is to understand and actually care for the patients…’
The students reflected upon how those competencies affect the patients’ experience of care and ultimately its outcomes.
12: ‘…I have also seen practices that might have made patients feel less welcome and less important, for which I will try to avoid doing during my service and practice as a future physician…’
32: ‘…the influence of doctor-patient dynamic on the delivery and outcomes of patient care…’
The students brought-up many skills with particular emphasis on interpersonal ones.
41: ‘…brings forth the importance of respect and autonomy…’
45: ‘…it teaches me crucial qualities that include empathy and teamwork…’
The importance of effective teamwork was (actually) repetitively alluded to.
32: ‘…allows medical students to understand the impact of effective teamwork in the clinical environment…’
Challenges
This category related to the difficulties in learning that the students experienced while participating in the ECE intervention.
12: ‘…there were several barriers to interacting with doctors. We were able to shadow nurses yet given that they were so focused on their work, they rarely engaged with us or supported us in learning about their systems and processes…’
Some of these difficulties were due to characteristics of the respective learning intervention. In other words, the ECE was designed in a particular way, with specific learning outcomes, which define and in turn limit its overall scope. For example, the students needed to commute to the placements and were meant to be in the authentic context of learning for a limited period of time.
2: ‘…we were there for a short time, and could not see and in turn learn much…’
6: ‘…during our visit, we barely saw any patients. I only saw the intake of one patient by a nurse…’
Some students offered suggestions for improving the logistics of the learning intervention. For example, providing the students with transportation was brought-up several times.
54: ‘…I suggest that transportation should be provided to the placements’ site…’
For some students, establishing the link between what they had observed as part of the ECE and their coursework was not a straightforward exercise.
4: ‘…it had not that much to do with the actual courses we are taking…’
The disparities in the learning experiences were also repetitively alluded to by the students as challenges to learning as part of the ECE.
30: ‘…from speaking to my colleagues, I can tell that my experience was far better than most of them, so not everyone was able to get the same insight into health care…’
Ultimately, the ECE is a direct reflection of the clinical environment, in terms of the activities that take place including but not limited to those relating to the patient flow. Variations in what the students get exposed to are inevitable..
44: ‘…experiences varied depending on the centers they visited and the time of the visit, so some might not have had the same opportunities as others…’
50: ‘…the disparity between my two visits underscores the variability in clinical exposures, emphasizing the importance of consistent, active engagement from our side for a comprehensive learning experience in medical education…’
Self-efficacy
This theme related to the students’ reflections of how the ECE increased their self-efficacy and in turn resilience in learning and in practicing medicine.
Motivation
This category encapsulated how the ECE contributed to increasing the students’ enthusiasm to engage more in their own learning as they are training to become future doctors.
22: ‘…it motivates us to keep-up with our studies…’
45: ‘…it helps boost motivation towards my studies as it shows me a glimpse of my future…’
ConfidenceS
This category highlighted the text segments that related to the students’ increased capacity of tolerating uncertainty.
10: ‘…it increases confidence in learning among students…’
31: ‘…feeling more confident and comfortable in a clinical setting…growing confidence upon better understanding patient needs and witnessing teamwork…’
The ECE was frequently described, in a way or another, as an ‘enabling experience’.
53: ‘…exposing us to several rounds of clinical history taking and consultation, which is quite enabling…’
Professional identity
This theme included all the ways by which the students describe the development of themselves in relation to the profession of medicine.
Purpose
This category related to how the students felt that the experience is reinforcing their ‘raison d'être’.
8: ‘…allowing us to meet patients face-to-face serves as a reminder of who we are studying all of this for so as not to become apathetic to disease and its impact…’
20: ‘…to understand what we are studying to become…’
Several students expressed that the ECE highlighted to them the significance of what they are after: their sense of purpose.
27: ‘…it shows me what my job will be as a healthcare practitioner all about…’
33: ‘…understanding the role of the doctor in the community…’
Several students emphasized that serving others appeared to be at the core of the profession of medicine. They appeared to have come to this realisation through observing that healthcare providers are constantly striving to ease patients’ pain.
16: ‘…it helped me know that this profession requires that I always ‘give it my all’, regardless of how many patients a doctor sees. Every patient deserves to be listened to, respected, and helped…’
The students saw firsthand how physicians realize their purpose.
42: ‘…realizing that everything we learn in lectures can contribute to one day treating a patient and easing their pain…’
Professionalism
This category related to the students’ reflections on the competencies and values that are shared among healthcare providers, in general, and physicians, in particular.
24: ‘…development of professional values and patient-centered care…’
54: ‘…… it helps in developing our professional identities by observing doctors interacting with their patients…’
The students emphasized the behaviours and attitudes that they consider ‘professional’.
15: ‘…it helps us envision the core values we need to be a successful doctor…’
44: ‘…learning to internalize and adopt the proper attitudes; observing effective communication skills early on will help us become more efficient, empathetic doctors moving forward…’
They also highlighted how the ECE enabled them to connect with and get to know role models who inspired them.
25: ‘…learning professional behaviour…very interesting, knowledgeable doctors…’
Foresight
The last theme included the students’ reflections of how the ECE raised their visibility in terms of their educational and professional trajectory.
Impression
This category showed that the ECE gave the students insight into their future careers, where they became better positioned in exploring and in turn identifying their interests.
16: ‘…it helps us see what we are interested in…’
The students highlighted how the ECE prepared them for upcoming stages.
34: ‘…giving us a glimpse at clinical life…’
38: ‘…getting a feel of interacting with real patients… develop insight into clinical practice…’
This learning experience shed light on the day-to-day work of doctors with particular emphasis on interacting with patients and striving to help others.
6: ‘…it gives us an idea of what our workdays will be like in the future…’
52: ‘…it gives me an idea of how I could help people if I were in the doctor’s place…’
Expectations
This category revolved around how the ECE enabled the students to manage their expectations.
29: ‘…helps us answer some of our future questions with regards to the specialities we would like to pursue…’
48: ‘…it orients us in terms of managing our expectations and setting professional standards…’
They associated the ECE experience with developing their personal and professional resilience.
7: ‘…the earlier we get used to clinical environment, the better we are at handling stress later during rotations and residency…’
8: ‘…sensitizing us to the general conditions of clinical care settings to minimize surprises when beginning our clinical learning in Year 4…’
Progression
This category related to descriptions of the progressive nature of the students’ learning and career trajectories.
11: ‘…a new introduction in my medical journey…’
47: ‘…ECE is a good step forward…’
The reflections of the students showed that they are clearly differentiating between early clinical exposure and learning in clinical environment.
13: ‘…learning in the clinical environment means hands-on learning in a real healthcare setting as opposed to a classroom or theoretical environment…’
32: ‘…being exposed to the clinical environment early on to understand the requirements needed for later years as medical students as well as the dynamic needed for our future careers…’
The students’ reflected on different upcoming steps.
10: ‘…make us better prepared to start clinical rotations in Year 4…’
44: ‘…throughout the subsequent years, we can build upon and refine this foundation…’
In terms of the value of the ECE, the students also differentiated between the short-term value which, according to them, related to preparing for learning in the clinical environment, and the long-term value which, to them, was about becoming better future physicians.
18: ‘…early clinical exposure provides immediate benefits like increased engagement in learning and observing for the betterment of communication skills
22: ‘…longer term effect of this early exposure is that it helps us to become better physicians…’
Integration
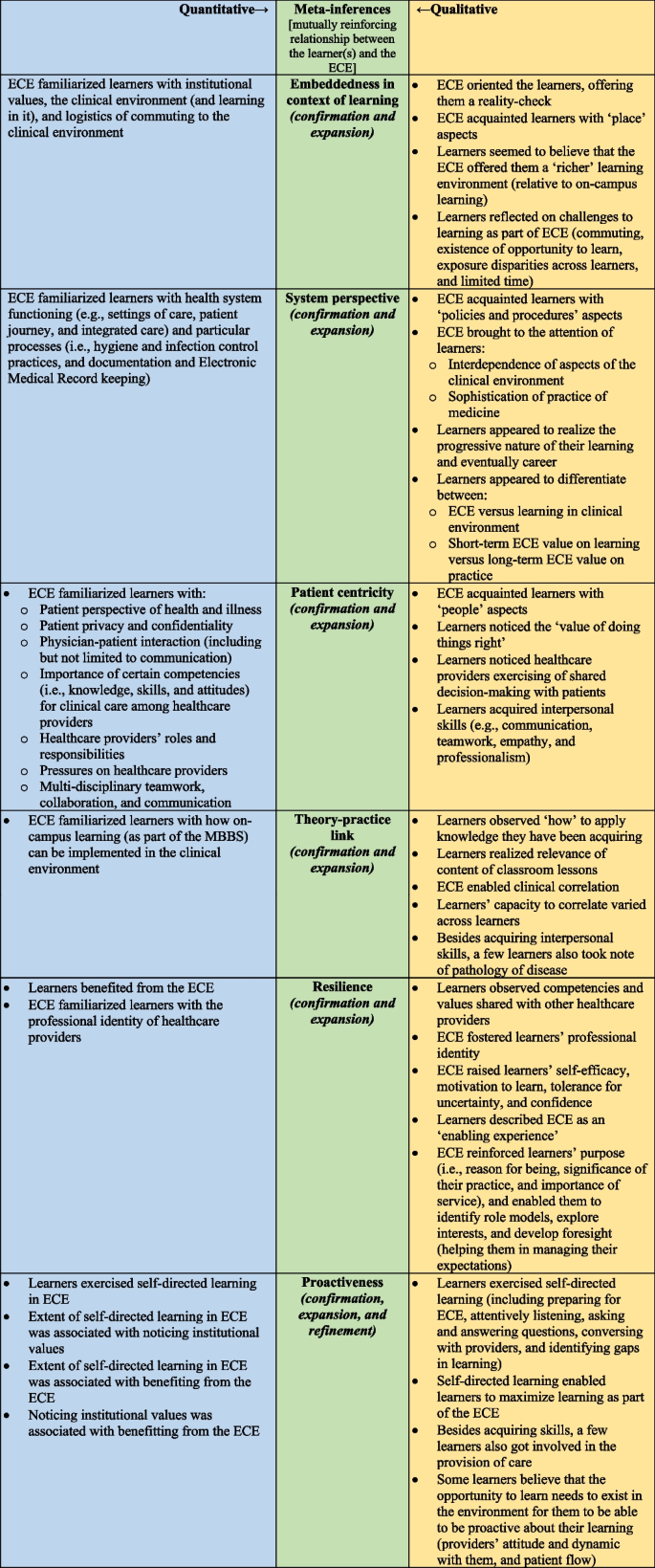
Integrating the output of the quantitative analyses with that of the thematic analysis revealed a holistic understanding of the learners’ perception of the subject matter, illustrated in the study’s side-by-side joint display (Fig. 6). The integration of findings (i.e., primary inferences) enabled the development of a thorough understanding of the learners’ experience with ECE. As such, integration led to six meta-inferences: Embeddedness in context of learning, System perspective, Patient-centricity, Theory–practice link, Resilience, and Proactiveness. There appeared to be a mutually reinforcing relationship—a virtuous cycle—between the learners and the learning integral to ECE across all six domains of the meta-inferences. In other words, the more committed the learners were to engage with any of the six domains, the more ECE advanced their progress in that direction.
Output of the iterative joint display analysis process, resulting in six meta-inferences: Embeddedness in context of learning, System perspective, Patient centricity, Theory–practice link, Resilience, and Proactiveness. The secondary color Green emerged by mixing the primary color Blue with the primary color Yellow (which constitutes an analogy of the lateral and critical thinking that took place to generate the meta-inferences from the integration of two sets of primary inferences). For the first five meta-inferences, integrating the quantitative with the qualitative inferences led to both: confirmation and expansion in the overall viewpoint. As for the last meta-inference, namely: Proactiveness, the integration led to: confirmation, expansion, and refinement of the overall viewpoint
The quantitative analyses indicated that the ECE helped learners become familiar with the clinical environment and the learning that occurs within it. Similarly, the qualitative analysis demonstrated that the ECE oriented learners to the context, providing them with a reality check. Additionally, the qualitative analysis revealed that students regarded learning in the clinical environment as ‘richer’ compared to the on-campus setting. The challenges associated with learning in the clinical environment were also clearly articulated by students in the narrative data. Thus, for the'Embeddedness in context of learning'meta-inference, the integration enabled both confirmation and expansion of the overall perspective.
For ‘System perspective’ meta-inference, the ECE helped learners understand how health systems function and the key processes involved. In line with this, the qualitative data analysis demonstrated that the ECE introduced learners to policies and procedures, highlighting how ‘the whole is greater than the sum of its parts’ in health system functioning. Furthermore, the qualitative analysis revealed the students’ awareness of the progressive nature of their learning and future careers. They appeared to clearly distinguish between the ECE and the subsequent learning they will undertake in Phase III of the MBBS, as well as the immediate value of the ECE for their current studies versus its long-term impact on their future clinical practice. This indicates that for the ‘System perspective’ meta-inference, the integration enabled both confirmation and expansion of the overall understanding.
For ‘Patient Centricity’ meta-inference, both the quantitative and qualitative analyses built upon each other. Each method underscored how the ECE acquainted learners with differing people-related aspects, including the importance of developing competencies that enhance patient care. The quantitative ratings reflected learners’ perceptions of distinct elements associated with interpersonal interactions, while the qualitative analysis demonstrated that, in addition to introducing learners to exemplary competencies displayed by healthcare providers, the observational aspect of the ECE helped them acquire a range of interpersonal soft skills. Thus, for the ‘Patient Centricity’ meta-inference, the integration led to both confirmation and expansion of the overall viewpoint.
Concerning the ‘Theory–practice link’ meta-inference, both qualitative and quantitative analyses indicated that the ECE exposed learners to how on-campus learning can be applied in the clinical environment. Moreover, the qualitative analysis revealed that the ability to make clinical correlations varied among learners. In addition to establishing connections related to interpersonal skills, some learners exceeded the intended learning outcomes by noting the pathology of diseases. Consequently, for the ‘Theory–practice link’ meta-inference, the integration once again resulted in both confirmation and expansion of the overall perspective.
In relation to the ‘Resilience’ meta-inference, the quantitative data showed that the learners benefited from the experience. Both the quantitative and qualitative analyses demonstrated that the learners observed competencies and values shared with other healthcare providers, which in turned fostered their professional identity. In addition, the qualitative analysis showed how the ECE further enabled the learners through raising their self-efficacy, motivation, tolerance, and confidence; reinforcing their purpose; identifying role models; exploring interests; and developing foresight. Accordingly, for the ‘Resilience’ meta-inference, the integration again led to both confirmation and expansion of the overall viewpoint.
Discussion
This study showed a mutually reinforcing relationship between the learners and the learning integral to the ECE in terms of embeddedness in the context of learning, system perspective, patient-centricity, theory–practice link, resilience, and proactiveness. Thus, the more the learners exercised any of the six abovementioned realms, the more ECE propelled them in the respective direction. This mutually reinforcing relationship may have become more pronounced due to anchoring the respective ECE in the complementarity of Kolb’s experiential learning theory with a social constructionism theory. It was suggested that ECE helps medical students socialize to their chosen profession {i.e., novices of any one professional group getting immersed in the professional culture; the process usually begins with getting acquainted with the professional roles [85]}. It helps them acquire a range of skills and makes their learning more authentic and relevant [86]. It was previously suggested that there are challenges in the delivery of basic sciences teaching that can be addressed through ECE [87]. These challenges encompass but are not limited to the lag in student participation, and the limited stimulation for further enquiry and exploration. Besides fostering greater student engagement, ECE tends to stimulate curiosity and inquiry, prompting students to delve deeper into topics of interest, thus fostering a culture of exploration and lifelong learning [87]. From this viewpoint, the ECE offers learning potential that learners can harness based on their level of proactivity, reflecting the saying: ‘the more you give, the more you receive’. It is established that higher levels of self-directed learning, in the clinical environment, are associated with higher academic achievement, more success in clinical skills, and better mental health outcomes (including anxiety and burnout) [21]. Yet, it is worth noting that a good proportion of the participating students articulated, in one way or another, the importance of having the opportunity to step up as a prerequisite for them to maximize their engagement. This highlights the importance of securing those engagement opportunities for the learners, as much as possible, when designing and planning for the ECE, and preparing all the relevant stakeholders for maximizing the learning experience [25]. It necessitates emphasizing, through capacity building, the educator role among the healthcare providers [18]. From personality psychology viewpoint, the degree of autonomy exhibited by students may be linked to their locus of control: essentially, their belief in whether they have control over the outcomes in their lives, as opposed to attributing those outcomes to external factors beyond their influence [88, 89]. Students who feel that they can maximize their learning experiences have an internal locus of control, while those who believe the advantages of education are dictated by external circumstances possess an external locus of control. Understanding these differences could be beneficial for medical educators, enabling them to create equitable learning opportunities that are tailored to the individual needs and preferences of medical students.
It is established that medical students tend to feel satisfied with and have positive attitude toward ECE [27]. It helps them in acclimatizing to clinical environments, developing professionally, and developing self-reflection and appraisal skill [86]. Along those lines, the current study introduced a novel conceptual model: ‘Early Clinical Exposure Added Value’, which brings forth undergraduate medical students’ perception of how the ECE benefitted them. This model can be deployed by medical educators in preparing students for learning in the clinical environment whether through ECE or otherwise. Operationalizing this model, as such, has the potential of enabling students to maximize their learning in the clinical environment. This shows how implementing ECE as part of MBBS at MBRU is feeding to local {e.g., Dubai Health- Care, Learning, and Discovery, and Giving [53, 54]}, national {e.g., Ministry of Higher Education and Scientific Research- Outcome-based Evaluation Framework [57]}, and international strategies and agendas {e.g., United Nations- SDGs 3, 4, and 9, and 17 [58]}. As such, the ECE has been adding value on micro-, meso-, and macro- levels [90, 91]. This study also introduced the'ECE Familiarization'tool, which was demonstrated to be both reliable and valid in the context of the study. This quantitative data collection instrument can also be utilized in other settings to evaluate educational clinical experiences.
The semi-quantitative tally around the output of the qualitative analysis indicates that participating students viewed the enabling of clinical correlations to be the most prominent benefit of the ECE, followed by gaining familiarity with characteristics of learning in the clinical environment, and then realizing the value of self-directed learning. Therefore, the most significant advantage of the ECE, as perceived by the students, appears to be its role in helping them understand how on-campus learning can be applied in a clinical context. In alignment with this, a prior literature review indicated that ECE sessions often motivate medical students, boost their confidence, improve academic performance, and enhance both clinical and communication skills. [7]. Additionally, it was suggested that ECE helps in diffusing stress associated with patient handling, developing clinical reasoning ability, enhancing assimilation and retention of knowledge, and improving communication skills, professional attitude, and empathy [26]. In a study focused on investigating the teaching of basic physiology to first-year MBBS students, it was found that ECE resulted in better knowledge retention and overall performance compared to traditional teaching methods. Most medical students involved in that study expressed their appreciation for the practical nature of ECE and described it as ‘more interesting’ [92].
In terms of embeddedness in the context of learning, the study clearly showed that the ECE familiarized learners with the clinical environment and learning in it, offering them a reality-check. It brought to their attention the challenges of learning in this environment. They got the chance to start experimenting with techniques to circumvent those challenges, or at least to entertain ideas in that direction. The latter might have happened consciously, or unconsciously given that as the saying goes: ‘what has been seen cannot be unseen’. The challenges that the students participating in the current study observed are similar to those previously indicated in the literature, such as: limited motivation to teach among the healthcare providers primarily due to competing responsibilities [45]. The literature also indicates challenges that were not brought-up in the current study, and these include: balancing clinical exposure with the rest of the workload in basic science education, patient confidentiality and safety, managing anxiety and stress, and addressing diversity and cultural competence [14]. Moreover, in terms of embeddedness in the context of learning of ECE, it would be valuable to foster the learning that occurs through interacting with others. This can happen through highlighting the importance of and encouraging, among the students, reflecting on the ECE experiences, and sharing of lessons learned and attained knowledge. Medical educators can go all the way to organize for structured debriefing sessions.
In relation to developing a system perspective, the ECE familiarized learners with health system functioning and key processes. It also refined the students’ understanding of the progressive nature of their learning and eventually career. A systematic literature review showed that ECE helps students learn about the structure and function of the healthcare system, and about preventive care and the role of health professionals [86]. In fact, the previously mentioned cross-sectional investigation across European medical schools, identified ‘gaining a holistic approach’ as one of the key learning objectives of ECE [93]. Another relevant mixed methods study showed that medical students articulated that ECE helped in preparing them for future years in medical school [94].
The ECE showed the students how patients remain at the core of healthcare delivery, the means by which all the people-related aspects feed into this core, and the significance of setting patient first as the core institutional value. ECE allows for active, experiential learning from patients along with practicing clinicians, designed to be the beginning of a lifelong learning focused on the patient [27]. This is particularly relevant when, similar to the context of the current study, the medical university is at the center of an academic health system [61]. This is in alignment with the key finding of a previously conducted systematic literature review that indicated: allowing students to gain a deeper understanding of the patient experience, and to develop empathy and a patient-centered approach to care, as the most prominent benefits of ECE [14]. Along those lines, it was previously suggested that ECE serves as a platform to orient students toward the social context of clinical practice, where it provides an opportunity to strengthen their cognitive and affective learning [94].
The ECE, reported upon in this study, built the learners’ resilience in several ways, including but not limited to: fostering their professional identity and self-efficacy, and developing foresight. Medical students tend to enjoy ECE, and to strongly agree that it raises their interest in learning and in turn academic performance [26]. It boosts their confidence in their own ability to succeed in medical practice [27]. It was previously suggested that ECE and the entailed interactions with the key stakeholders (including patients and their families) enable students to form and cultivate a sense of medical professionalism [95]. A qualitative study of medical students in Taiwan indicated the specific medical professionalism domains that were reinforced through ECE. These include: medical knowledge and clinical skills; interpersonal skills with patients; teamwork; duty towards public health; and protection of patients’ rights [9]. It was suggested that ECE supports fresh medical students in overcoming their stresses [96], and motivates them to develop better insight and awareness to the medical profession [27, 97]. In addition, a previously conducted investigation, around ECE in Debra Tabor University in Ethiopia, showed that the students considered the respective ECE to have played a key role in developing their professional knowledge, enhancing their problem-solving abilities, increasing their motivation, encouraging them to be proactive about their own learning, and fostering a community orientation among them [45].
Developing the ECE, reported upon in this study, through design-based research enabled understanding the undergraduate medical students’ needs and proactively addressing them [40]. The iterative process of design-based research allowed for the optimization of the design of the ECE. Design-based research also enabled striving for both practical and theoretical outcomes [39]. Besides their practical added value on the students, the firsthand experiences of the ECE revealed the value that resulted from grounding the intervention in experiential learning theories [31, 32]. Several previously conducted studies have reported on examples of ECE which were anchored in Kolb’s experiential learning theory [26, 27]. In principle, doing so substantiates the intervention. Yet, relying solely on Kolb’s experiential learning theory may result in overlooking the learning that occurs in relating to others. In fact, it was previously suggested that even without specific educational interventions, by simply placing students in a nurturing social environment, their motivational self-regulation skills are enhanced [20]. Hence, the firsthand experiences reported upon in the current study sheds light on the value of basing the ECE on the complementarity of Kolb’s experiential learning theory with a social constructionism theory (where a small group of people learn through their social interactions) [38]. This brings experiential learning back to its origins, where it stemmed from human relations’ training [34], and conceptualizes experiential education in more sociological terms, showing that the individual learner is certainly connected to social, cultural, and/or environmental factors [36]. It also emphasizes, in alignment with the findings of this study, that participation and learning go together, and that the learner is embedded in the context of learning.
This study has a few limitations. Choosing to address the overall purpose of this study using mixed methods approach allowed for the generation of transferable insights. However, the generalizability of the findings is limited to contexts similar to that of MBRU. The sample size was small, covering a single cohort of undergraduate medical students only. Accordingly, further investigations around ECE are needed; these can be with greater numbers of students, longitudinal, and/or using diverse data collection tools. It will be worthwhile for future studies to include several medical colleges, and/or cohorts within the same college. In addition, while ECE is evolving based on the current research, a significant gap remains in evaluating its long-term impact, particularly in terms of improving clinical skills and professionalism [14]. Such a long-term evaluation is crucial for understanding whether ECE leads to sustained improvements in medical practice and professional behavior, making it an essential area for future exploration in medical education.
Conclusion
This study indicates that ECE holds a learning potential that is realized by the medical students, depending on their proactivity. The more the learners embed themselves in the context of learning, the more the ECE contributed to building their academic resilience, and propelled them in terms of clinical correlations, skills’ development, and values reinforcement. Securing engagement opportunities for the learners, when designing and planning for the ECE, is essential. Optimizing the ECE learning value, as such, can happen systematically through continuously developing the respective intervention in alignment with the principles of design-based research and anchoring it in constructivism experiential learning theories.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Deml MJ, Jungo KT, Maessen M, Martani A, Ulyte A. Megatrends in Healthcare: Review for the Swiss National Science Foundation’s National Research Programme 74 (NRP74) “Smarter Health Care.” Public Health Rev. 2022;43:1604434.
J.R. F: The CanMEDS 2005 Physician Competency Framework. Better standards. Better physicians. Better care. In. Edited by Canada OoETRCoPaSo. Ottawa: The Royal College of Physicians and Surgeons of Canada.; 2005.
Senok AJBA, Al Heialy S, Naidoo N, Otaki F, Davis D. Leveraging the Added Value of Experiential Co-Curricular Programs to Humanize Medical Education. Journal of Experiential Education. 2022;45:172–90.
Otaki F, Naidoo N, Al Heialy S, John-Baptiste AM, Davis D, Senok A. Shaping the future-ready doctor: a first-aid kit to address a gap in medical education. Int J Med Educ. 2020;11:248–9.
Ninan D, Patel D. Career and Leadership Education in Anesthesia Residency Training. Cureus. 2018;10(4):e2546.
White CP, Lecours C, Bortoluzzi P, Caouette-Laberge L, Ying Y. International plastic surgery missions: a framework for resident education using the CanMEDS competencies. Ann Plast Surg. 2013;71(4):324–7.
Tayade MC, Latti RG. Effectiveness of early clinical exposure in medical education: Settings and scientific theories - Review. J Educ Health Promot. 2021;10:117.
Dornan T. Osler, Flexner, apprenticeship and ‘the new medical education.’ J R Soc Med. 2005;98(3):91–5.
Liu CI, Tang KP, Wang YC, Chiu CH. Impacts of early clinical exposure on undergraduate student professionalism-a qualitative study. BMC Med Educ. 2022;22(1):435.
von Below B, Hellquist G, Rodjer S, Gunnarsson R, Bjorkelund C, Wahlqvist M. Medical students’ and facilitators’ experiences of an Early Professional Contact course: active and motivated students, strained facilitators. BMC Med Educ. 2008;8:56.
RA S. Perception of Early Clinical Exposure (ECE) among Phase I MBBS Students in a Medical College in Northeastern India. Journal of Medical Sciences. 2024;10:169.
Ebrahimi SKJ, Ashkani ES. Early clinical experience: A way for preparing students for clinical setting. Galen Medical Journal. 2012;1(2):42–7.
Sawant SP, Rizvi S: Early Clinical Exposure (ECE) as an Effective Learning Tool in Anatomy. 2023.
Ingale MH, Tayade MC, Bhamare S. Early clinical exposure: Dynamics, opportunities, and challenges in modern medical education. J Educ Health Promot. 2023;12:295.
Sekkizhar U, Ramanathan R, Sakthivel PA, Shanmugam J. Effectiveness of early clinical exposure in competency-based curriculum–A step forward. National Journal of Physiology, Pharmacy and Pharmacology. 2024;14(1):27–32.
Kane T, Chivese T, Al-Moslih A, Al-Mutawa NAM, Daher-Nashif S, Hashemi N, Carr A. A program evaluation reporting student perceptions of early clinical exposure to primary care at a new medical college in Qatar. BMC Med Educ. 2021;21(1):162.
Khanal S, Bhusal M, Sigdel M, Bajracharya S: Acquisition of history taking, physical examination and communication skills through early clinical exposure among pre-clinical students. Journal of Institute of Medicine Nepal (JIOMN) 2015;37(3).
Maheshwari K, Shigli K, Tiwari B, Bukya D, Oberoi SS, Ansari MWF, Mondal T. Introduction and Effectiveness of Early Clinical Exposure Among Dental Students in Pre-clinical Prosthodontics. Cureus. 2024;16(8):e66126.
Kumar P, Mythri G, Shetty A, Yashaswini L, Chaitra N. First-year medical students’ perspective on early clinical exposure in the era of competency-based medical education: unraveling by thematic analysis. Medical Journal of Dr DY Patil University. 2023;16(3):322–8.
Salajegheh M, Rooholamini A, Norouzi A. Investigating the role of clinical exposure on motivational self-regulation skills in medical students based on cognitive apprenticeship model. BMC Med Educ. 2024;24(1):257.
Cho KK, Marjadi B, Langendyk V, Hu W. The self-regulated learning of medical students in the clinical environment - a scoping review. BMC Med Educ. 2017;17(1):112.
Yadav SPP, Pasricha N, Bhatnagar R. Assessing the role of early clinical exposure in anatomy: a perception and feedback. Int J Adv Res. 2024;12:1499–507.
Singh RA. Perception of Early Clinical Exposure (ECE) among Phase I MBBS Students in a Medical College in Northeastern India. J Med Sci. 2024;10(2):169.
Lee H.Y. IS, Shin S.W., Kim J.A., Song J.M.: Effect of Early Clinical Exposure based Health Systems Science course in the Korean Medical Education: A Prospective Observational Study. Research Square 2024.
Fisher J, Foggin J, Paes P: Provision of early clinical experience in UK medical schools: a cross-sectional survey. Educ Prim Care 2024:1–9.
Tayade MC, Giri PA, Latti RG. Effectiveness of early clinical exposure in improving attitude and professional skills of medical students in current Indian medical education set up. J Family Med Prim Care. 2021;10(2):681–5.
Warkar AB. AAA: Introduction to early clinical exposure as learning tool in physiology. Indian J Physiol Pharmacol. 2021;64:S62–9.
Panadero E. A Review of Self-regulated Learning: Six Models and Four Directions for Research. Front Psychol. 2017;8:422.
Zimmerman B.J. MAR: Self-regulation: Where metacognition and motivation intersect. In: In Handbook of metacognition in education. edn.: Routledge; 2009: 299–315.
Zigmont JJ, Kappus LJ, Sudikoff SN. Theoretical foundations of learning through simulation. Semin Perinatol. 2011;35(2):47–51.
Wijnen-Meijer M, Brandhuber T, Schneider A, Berberat PO. Implementing Kolb s Experiential Learning Cycle by Linking Real Experience, Case-Based Discussion and Simulation. J Med Educ Curric Dev. 2022;9:23821205221091510.
S.P. G: Integrating the experiential learning cycle with educational supervision. Journal of Educational Supervision 2022, 5.
Yardley S, Teunissen PW, Dornan T. Experiential learning: transforming theory into practice. Med Teach. 2012;34(2):161–4.
DU Seaman J, Humberstone B, Martin B, Prince H, Quay J. Joint recommendations on reporting empirical research in outdoor, experiential, environmental, and adventure education journals. Journal of Experiential Education. 2020;43:348–64.
Barab S. SK: Design-based research: Putting a stake in the ground. In: Design-based Research. edn. Edited by Press P; 2016: 1–14.
BdC C. Theory and praxis in experiential education: some insights from gestalt therapy. Journal of Experiential Education. 2020;43:156–70.
Junhua L. ZY, Ruths J., Moreno D., Jensen D.D., Wood K.L.: Innovations in software engineering education: An experimental study of integrating active learning and design-based learning. In: ASEE Annual Conference & Exposition. 2013: 23–758.
J Q. Experience and participation: Relating theories of learning. Journal of Experiential Education. 2003;26:105–12.
McKenney S, Reeves TC. Educational design research: Portraying, conducting, and enhancing productive scholarship. Med Educ. 2021;55(1):82–92.
Chen W, Reeves TC. Twelve tips for conducting educational design research in medical education. Med Teach. 2020;42(9):980–6.
Kimmons R. Current Trends (and Missing Links) in Educational Technology Research and Practice. TechTrends. 2020;64(6):803–9.
Kimmons R. CS: The Students' Guide to Learning Design and Research; 2020.
Sandars J, Goh PS. Design Thinking in Medical Education: The Key Features and Practical Application. J Med Educ Curric Dev. 2020;7:2382120520926518.
Dolmans DH, Tigelaar D. Building bridges between theory and practice in medical education using a design-based research approach: AMEE Guide No. 60. Med Teach. 2012;34(1):1–10.
Ewnte B, Yigzaw T. Early clinical exposure in medical education: the experience from Debre Tabor University. BMC Med Educ. 2023;23(1):252.
KOF Globalisation Index [https://kof.ethz.ch/en/forecasts-and-indicators/indicators/kof-globalisation-index.html].
Alameddine M, AlGurg R, Otaki F, Alsheikh-Ali AA. Physicians’ perspective on shared decision-making in Dubai: a cross-sectional study. Hum Resour Health. 2020;18(1):33.
Alameddine M, Otaki F, Bou-Karroum K, Du Preez L, Loubser P, AlGurg R, Alsheikh-Ali A. Patients’ and physicians’ gender and perspective on shared decision-making: A cross-sectional study from Dubai. PLoS ONE. 2022;17(9):e0270700.
Levitt HM, Bamberg M, Creswell JW, Frost DM, Josselson R, Suarez-Orozco C. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73(1):26–46.
Transformative learning at Mohammed Bin Rashid University of Medicine and Health Sciences [https://www.mbru.ac.ae/].
Facts and figures [https://www.mofa.gov.ae/en/the-uae/facts-and-figures].
Connected for you [https://dubaihealth.ae/].
About Dubai Health [https://dubaihealth.ae/about-dubai-health#:~:text=We%20serve%20to%20impact%20lives%20and%20shape%20the,Values%20Patient%20First%20Respect%20Excellence%20Teamwork%20Integrity%20Empathy].
Dubai Health Authority [https://www.dha.gov.ae/en/AboutUs].
Wartman S. The Transformation of academic health centers: meeting the challenges of healthcare’s changing landscape. London: Academic Press, an imprint of Elsevier; 2015.
Research MoHEaS: Outcome-based Evaluation Framework. In. Edited by Universities EFaRMf. Abu Dhabi, United Arab Emirates: Ministry of Higher Education and Scientific Research; 2025.
Nations U: The 2030 Agenda for Sustainable Development. In. Edited by Affairs DoEaS; 2015.
Queen's University Belfast [https://www.qub.ac.uk/].
Otaki F, AlHashmi D, Khamis AH, Azar AJ. Investigating the evolution of undergraduate medical students’ perception and performance in relation to an innovative curriculum-based research module: A convergent mixed methods study launching the 8A-Model. PLoS ONE. 2023;18(1):e0280310.
Du Preez L. OF, Clemens T., Al-Hammadi S., Stanley A., Ho S.B., Kilian P., Loubser P., Bayoumi R., Ezimokhai M., Bedford B., Fathey T., AlGurg R., Al Suwaidi H., Sharif A.A., Alsheikh-Ali A.A.: A values-driven academic affiliation between a public medical school and a private healthcare provider: exploring the perceptions of key opinion leaders. Research Square 2024.
Mediclinic Middle East (MCME) [https://www.mediclinic.ae/en/corporate/home.html].
Khalaf Ahmad Al Habtoor Medical Simulation Center [https://www.mbru.ac.ae/learning-resources/khalaf-ahmad-al-habtoor-medical-simulation-center/].
Guetterman TC, Fetters MD, Creswell JW. Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research Through Joint Displays. Ann Fam Med. 2015;13(6):554–61.
MD F: The Mixed Methods Research Workbook: Activities for Designing, Implementing, and Publishing Projects: Thousand Oaks: SAGE Publications, Inc.; 2020.
Jackson L, Otaki F. Using team-based learning to optimize undergraduate family medicine clerkship training: mixed methods study. BMC Med Educ. 2023;23(1):422.
Otaki F, Amir-Rad F, Al-Halabi M, Baqain Z, Zary N. Self-reported adaptability among postgraduate dental learners and their instructors: Accelerated change induced by COVID-19. PLoS ONE. 2022;17(7):e0270420.
Kaddoura R, Faraji H, Otaki F, Radhakrishnan R, Stanley A, Paulus A, Jackson L, Al Jayyousi R, Mascarenhas S, Sudhir M, et al. High-fidelity simulation versus case-based tutorial sessions for teaching pharmacology: Convergent mixed methods research investigating undergraduate medical students’ performance and perception. PLoS ONE. 2024;19(8):e0302609.
Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–56.
Molina-Azorin JFFM. Building a Better World Through Mixed Methods Research. J Mixed Methods Res. 2019;13:275–81.
Boet S, Sharma S, Goldman J, Reeves S. Review article: medical education research: an overview of methods. Can J Anaesth. 2012;59(2):159–70.
Roberts C: Mixing modes of data collection in surveys: A methodological review. 2007.
Nayak M, Narayan K. Strengths and weaknesses of online surveys. Technology. 2019;6(7):0837–2405053138.
Explorance Blue: The next-generation feedback analytics platform [https://www.explorance.com/products/blue].
The People Insights Platform [https://explorance.com/products/blue/].
K Y. Comparison of Quantitative and Qualitative Research Traditions: epistemological, theoretical, and methodological differences. European journal of education. 2013;48:311–25.
Stiles WB. Quality control in qualitative research. Clin Psychol Rev. 1993;13(6):593–618.
Va BVAC. Using thematic analysis in psychology. Qualitative research in psychology. 2006;3:77–101.
Braun V, Clarke V. Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol Rev. 2023;17(4):695–718.
Nair B, Otaki F, Nair AF, Ho SB. Medical students’ perception of resilience and of an innovative curriculum-based resilience skills building course: A participant-focused qualitative analysis. PLoS ONE. 2023;18(3):e0280417.
Buhumaid R, Otaki F, Czabanowska K, Stanley A, Ezimokhai M, Jackson L, Ho SB. Professionalism-training in undergraduate medical education in a multi-cultural, multi-ethnic setting in the Gulf Region: an exploration of reflective essays. BMC Med Educ. 2024;24(1):117.
NVivo 15 - The Most Trusted Qualitative Analysis Software (QDA) is Even Better [https://lumivero.com/products/nvivo/].
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51.
Dossett LA, Kaji AH, Cochran A. SRQR and COREQ Reporting Guidelines for Qualitative Studies. JAMA Surg. 2021;156(9):875–6.
Salisu WJ, Dehghan Nayeri N, Yakubu I, Ebrahimpour F. Challenges and facilitators of professional socialization: A systematic review. Nurs Open. 2019;6(4):1289–98.
Dornan T, Littlewood S, Margolis SA, Scherpbier A, Spencer J, Ypinazar V. How can experience in clinical and community settings contribute to early medical education? A BEME systematic review Med Teach. 2006;28(1):3–18.
Yadav SKPAR, Sethi Y. Shaping future healers: The impact and implementation of Early Clinical Exposure in medical education. Indian Journal of Forensic and Community Medicine. 2024;11:1–4.
Szabó-Morvai Á. KHJ: Locus of control, educational attainment, and college aspirations: the relative role of effort and expectations. Educ Econ. 2024;32:862–81.
M K. A review of classical motivation theories: A study understanding the value of locus of control in higher education. Journal of Interdisciplinary Studies in Education. 2018;7:34–53.
Borg N, Naderpajouh N, Scott-Young CM, Borg J. An interdisciplinary and multi-level review of resilience to inform training of human resources for critical infrastructure. International Journal of Disaster Risk Reduction. 2022;78:103113.
Msosa WH. Records management practices at the Northern region water board. Malawi: Mzuzu University; 2022.
Das P, Biswas S, Singh R, Mukherjee S, Ghoshal S, Pramanik D. Effectiveness of early clinical exposure in learning respiratory physiology among the newly entrant MBBS students. J Adv Med Educ Prof. 2017;5(1):6–10.
Simmenroth A, Harding A, Vallersnes OM, Dowek A, Carelli F, Kiknadze N, Karppinen H. Early clinical exposure in undergraduate medical education: A questionnaire survey of 30 European countries. Med Teach. 2023;45(4):426–32.
SinghKharay SVH, Puri S, Bansal P. Phase I Medical Students’ Perceptions of Early Clinical Exposure In Classroom and Hospital Setting: A Qualitative and Quantitative Analysis. Future Health. 2023;1:8–14.
Martin EM, Handlos JL, Ludwig G. Implementation and Evaluation of an Interprofessional Education Workshop to Enhance Health Care Student Resilience and Adaptability. Athl Train Educ J. 2023;18(1):33–40.
Hackey R. Fostering Resilience in Experiential Learning Courses. Experiential Learning and Teaching in Higher Education. 2023;6(1):13–23.
Xu Y, Zhang W, Wang J, Guo Z, Ma W: The effects of clinical learning environment and career adaptability on resilience: A mediating analysis based on a survey of nursing interns. Journal of Advanced Nursing 2024.
Acknowledgements
The principal investigator would like to thank the MBRU faculty members and clinicians who contributed to delivering the content of Foundation of Clinical Medicine 2 (FOCM2) course and Early Clinical Exposure (ECE) investigated in the current study. In addition, the authors would like to extend gratitude to MBRU Research and Graduate Studies academic unit for supporting this research work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
R.A.J.- Coordinated the Foundation of Clinical Medicine 2 (FOCM2) course and designed the Early Clinical Exposure (ECE) intervention reported upon in the current research study; maintained the macro perspective of the current research study; contributed to development of data collection tool; analyzed the data; and composed and submitted the final submission of the manuscript. N.A.- Co-coordinated the FOCM2 course and contributed to the delivery of the ECE reported upon; contributed to development of data collection tool; and contributed to the final version of the manuscript. F.O.- Contributed to development of data collection tool; analyzed the data; and composed the final version of the manuscript. A.P.- Contributed to the final version of the manuscript. K.C.- Contributed to the final version of the manuscript. Q.Z.- Organized the student allocations to placements and administration of the ECE intervention reported upon; contributed to development of data collection tool; and contributed to the final version of the manuscript. M.A.- Contributed to the final version of the manuscript. A.S.- Contributed to the final version of the manuscript and edited prepared Figs. 2 and 3. P.K.-Coordinated the ECE placements; contributed to development of data collection tool; and contributed to the final version of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study adhered to the Declaration of Helsinki. It was approved by two relevant research governing entities: Institutional Review Board of MBRU (MBRU IRB- 2024–20) and Dubai Scientific Research and Ethics Committee (DSREC) at the DHA (DSREC-GL14 - 2024). The research participants gave their informed consent electronically prior to filling in the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Al-Jayyousi, R., Abu Mahfouz, N., Otaki, F. et al. Investigating the learning value of early clinical exposure among undergraduate medical students in Dubai: a convergent mixed methods study. BMC Med Educ 25, 638 (2025). https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12909-025-07212-9
Received:
Accepted:
Published:
DOI: https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12909-025-07212-9
Keywords
- Early clinical exposure
- Basic medical sciences
- Foundation of clinical medicine
- Clinical medical sciences
- Self-regulation
- Self-directed learning
- Clinical correlation
- Resilience
- Resilient health professionals
- System perspective
- Patient first
- Patient centricity
- Undergraduate medical education
- Medical education
- Health professions education
- Align
- Alignment
- Learning
- Care
- Discovery
- Giving
- Dubai
- Dubai Health
- Outcome-based Evaluation Framework
- Ministry of Higher Education and Scientific Research
- United Arab Emirates
- Sustainable Development
- Sustainable Development Goals
- SDG 3
- SDG 4
- SDG 9
- SDG 17
- United Nations
- Design
- Based research
- Adult learning theory
- Kolb’s experiential learning theory
- Social constructionism
- Mixed methods research